It is crucial that sufferers receive support from families, friends, and communities

The situation of mental health in Nepal remains dismal. The prevalence of mental health disorders in the general population is 37.5 percent, but the ratio of mental health care service providers is about 0.22 per 100,000 population. Political instability, economic woes, earthquakes and many other disasters have taken a severe toll on the mental health condition of the Nepali population. Besides, a culture of silence surrounding the symptoms of mental illness has a strong bearing on access to available healthcare services in Nepal.
Increasing stigmatisation of mental illness has prevented an understanding of the social and biological causes of mental disorders. One of such mental disorders is schizophrenia. Unfortunately, there is little evidence or research that shows the prevalence of the illness in Nepal. A study conducted in Janakpur and a tertiary care mental hospital in Kathmandu showed a high prevalence of 30 percent reporting schizophrenia symptoms. More evidence and advanced research on schizophrenia can create situations to address mental health in the country.
The symptoms
How an individual thinks, feels and behaves indicates the symptoms of schizophrenia, and these processes vary among individuals. Some have strange or false beliefs and unclear or confused thinking, others hear voices that are not there (hallucination), have agitated body movements, exhibit poor social interaction, feel less expressive, and have reduced feelings of pleasure in everyday life. They could also have difficulties beginning and sustaining activities and have trouble focusing or paying attention. Schizophrenia is not as common as other mental disorders, but the symptoms can be very disabling—not only to the individual but also to families. Family members face the burden of care, fear and embarrassment, and the lack of social support and stigma.
The high cost of treatment, lack of medical facilities, and inadequate human resources are compounding the problems of the mental health care system in Nepal. This has led to the stigmatisation of the illness, ostracisation of individuals and families manifested through the loss of income and employment, increased expenses, reduced productivity, reduced quality of life, emotional strain and disturbed social relations.
There are many such cases where people within urban centres, such as the Kathmandu Valley, are not aware of how disabling mental disorders can be. The stigmatisation of people with mental disorders forces them to hide either their symptoms or the symptoms of a family member with the hope that they will pass away. Such individuals are forced to get married or have children thinking that it could cure their mind without realising that this could make their life more miserable. Thus, people with schizophrenia are likely to neglect or harm themselves, and global evidence indicates that one in 10 people commit suicide.
There are lessons to be learned from societies globally that offer programmes and services to support, educate, engage and empower individuals, families and communities impacted by schizophrenia and psychotic illness. Such societies not just help raise awareness about how crippling mental health disorders can be, but also help lift the quality of life for those who suffer from them.
In today’s society, people become ill with schizophrenia when they should be developing technical skills and pursuing a career. It is crucial that they receive support from their families, friends and communities with the first onset of symptoms such as having difficulty working with other people. The first time a person experiences symptoms of schizophrenia can be made worse with loneliness.
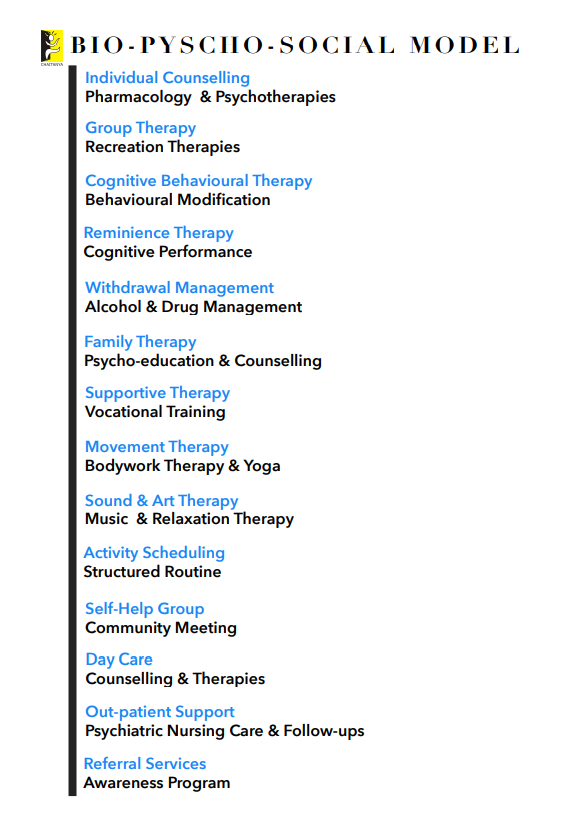
To address such issues and problems, consideration of the social and biological causes of mental disorders is a prerequisite, along with antipsychotic medication. Psychological therapy, family therapy and occupational training are few of such bio-psycho-social models that help understand the specific needs of individuals for reintegration. Recognition of such models within policies and health care priorities will support the government’s efforts to improve the framework for mental health in Nepal.
Widespread misconception
Despite the widespread misconception that people with schizophrenia have no chance of recovery or improvement, there is hope. Although there is currently no cure for schizophrenia, it can be treated and managed with medication, self-help strategies and supportive therapies. One can have more control over recovery than one probably realises.
Believing in coping with schizophrenia is a lifelong process. Therefore, recovery does not mean one will not experience any more challenges from the illness or that one will always be symptom-free. It is necessary to support individuals to manage their symptoms, develop the support they need, and create a satisfying, purpose-driven life. A well-designed treatment plan that combines medication with self-help, supportive services and therapy is the most effective approach.
Bastola is the director of the Chaitanya Institute for Mental Health, Nepal
https://kathmandupost.com/opinion/2019/05/24/schizophrenia-in-nepal
Leave a Reply